What Is Coronavirus and How Do Humans Defeat It?
Accompanying worldwide awareness of the COVID–19 pandemic is an understandable fear of the disease as well as misunderstandings of what causes it. Microscopic germs, invisible to the naked eye and which can spread silently from person to person, are the cause of this infectious disease.
As of April 2020, there is no proven treatment or ‘cure’ for coronavirus infections. The best prevention against contracting the virus is to wash one’s hands with soap after touching public surfaces, as well as to refrain from touching one’s eyes, nose and mouth — points of entry for the virus.

Lately, President Trump has been enthusiastically urging people to self-medicate with a chemical called hydroxychloroquine, a drug prescribed for malaria patients as well as those afflicted with lupus. Despite no scientific evidence that hydroxychloroquine prevents COVID–19, Trump has been insisting that there are “some very strong signs” that the drug is an effective preventative measure.
Doctor Radha Rajasingham works as an assistant physician for the University of Minnesota’s Medical School, Infectious Diseases and International Medicine division (UMN). She and her team have been performing clinical trials on the effectiveness of hydroxychloroquine against contracting COVID–19.
The drug is thought to disrupt the method by which coronaviruses SARS-CoV and SARS-CoV-2 attach themselves to host cells inside of a person’s airways. Hydroxychloroquine is not a vaccine against COVID–19 nor a treatment for a person already infected with the new coronavirus.
Watch Dr. Rajasingham’s interview with MEGA:
Below we have detailed some of the science and history behind viral and bacterial infections, as well as other ongoing research regarding battling the new coronavirus.
Historical study of the invisible enemy
The term ‘epidemic’ was first used in a medical sense around the turn of the fourth century B.C. in reference to the appearance of a collection of illness symptoms that occurred in people in the same area at the same time.
In the 11th century A.D., Persian physician Ibn Sina wrote on epidemics, noting that tuberculosis could be transmitted from person to person via breath or through contaminated water or dirt. His medical encyclopedia, The Canon of Medicine (Al-Qanun fi’t-Tibb), was used as the standard medical textbook by Islamic and European medical practitioners for almost 700 years.
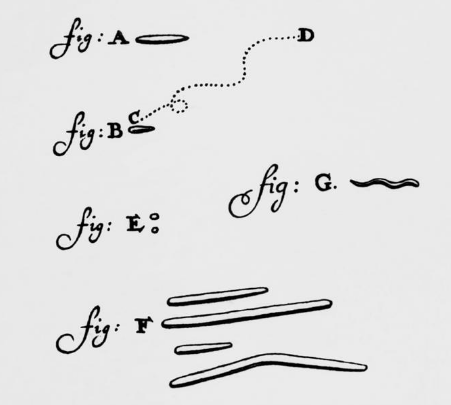
Germs — tiny disease-causing organisms or ‘microbes’ invisible to the naked eye — had been suspected for well over a thousand years by various cultures. However, direct evidence wasn’t possible until the invention of the optical microscope in 1676, when bacteria (single-celled organisms) were observed for the first time by Dutch microscopist Antonie van Leeuwenhoek.
It took another 200 years before European scientists accepted the notion that microbes cause disease, known as ‘germ theory.’
Belief in the unseen
Before germs were well-known as agents of illness, it was believed that foul odors or ‘bad air’ emitted from decaying organic matter caused disease; this was ‘miasma theory.’
In the 1840s, physician Ignaz Semmelweis demonstrated that patient mortality rates were drastically reduced by the simple act of a medical practitioner sanitizing their hands before touching a new patient. He had doctors first wash their hands with soap then with a bleach solution, which removed not only unpleasant odors but also the bacteria that lingered unseen.
The three decades following the late 1850s saw a shift in European medical opinion away from miasma theory due to the revelations of several scientists.
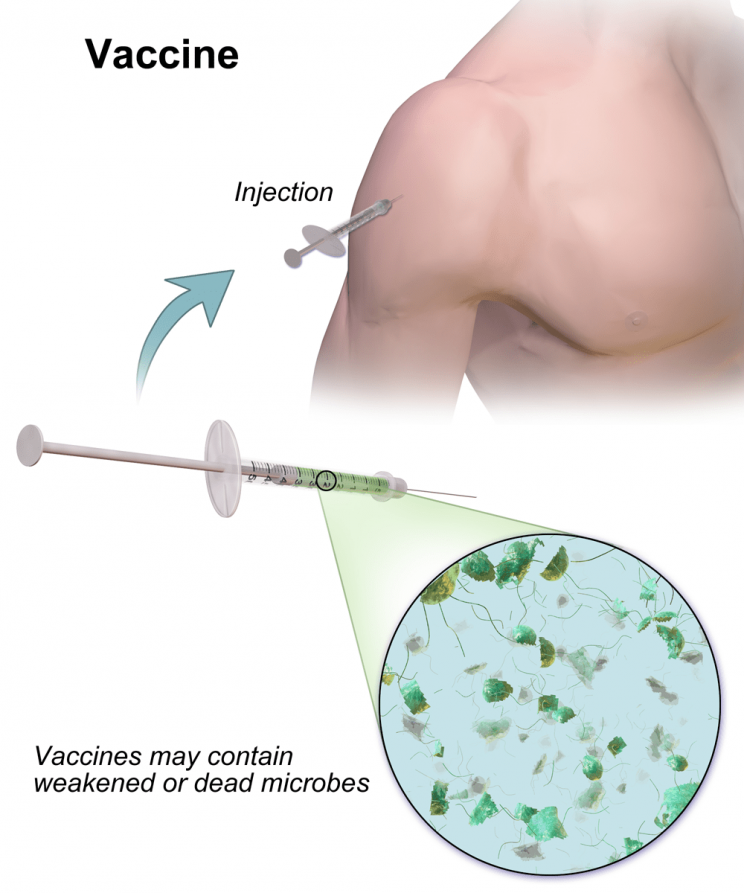
Notable among those scientific contributions are those of Robert Koch, who demonstrated that a given disease is caused by a specific organism, and Louis Pasteur, who developed some of the world’s first vaccines. A ‘vaccine’ is a sample of weakened microbes that, when introduced inside a host’s body, cause an immune system response that protects the body against future full-strength microbes of the same type.
By the 1890s, the miasma theory of contagion had been supplanted by germ theory. Around this time, viruses, infectious particles much smaller than bacteria, were also discovered.

Pathogens infecting pathogens
Both bacteria and viruses can be ‘pathogens,’ biological substances that cause disease in plants and animals. Unlike a bacterium, a ‘virion’ (an individual virus particle) cannot reproduce outside of a living host.
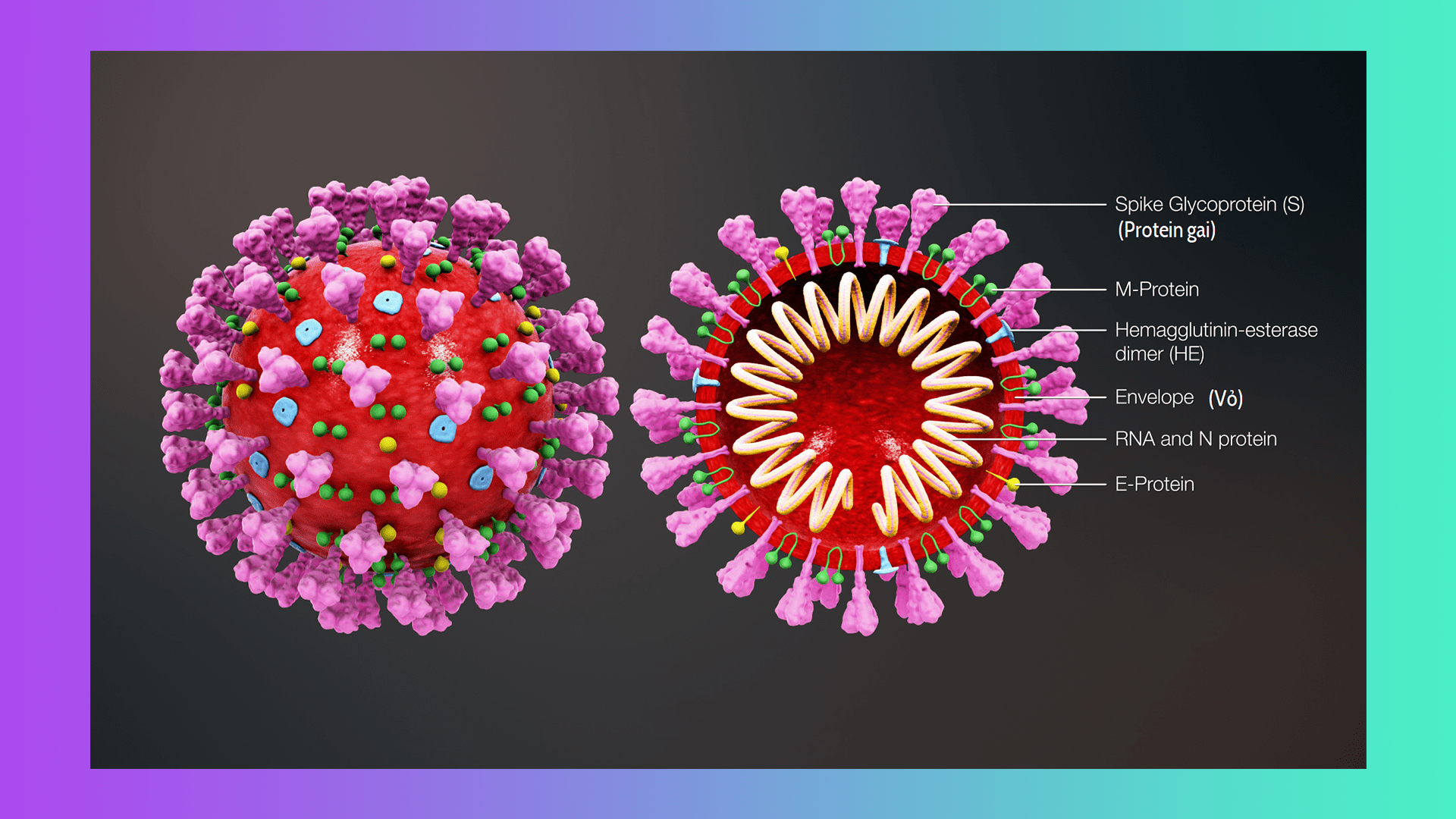
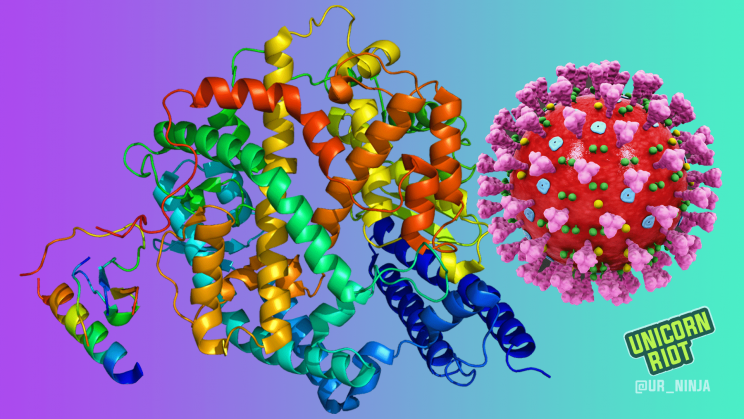
Virions are the most abundant biological entities on Earth and can infect bacteria and fungi in addition to plants and animals. They consist of genetic material as well as polymerase enzyme — complex structures that help copy the genome — all wrapped in protein coating(s).
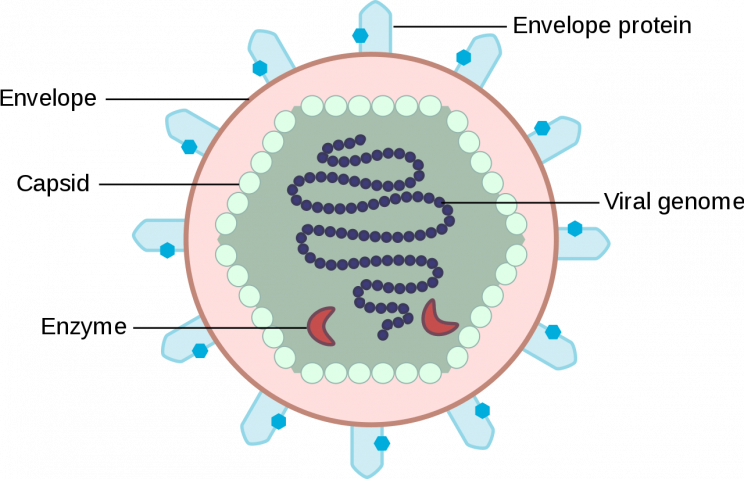
Virus particles reproduce by attaching themselves to a living cell, penetrating the cell wall, and releasing genetic material inside the host cell. The virus then uses the host cell to manufacture and assemble copies of itself, virions which burst forth or are otherwise released from the host cell.
Most viruses are about a hundred times smaller than bacteria and cannot be seen through an optical microscope. It was not until the invention of the electron scanning microscope in the 1930s that the first high-resolution images of viruses became available.
Combating the invisible
Antibiotics, drugs that kill bacteria cells but leave the body’s own cells unharmed, had been in use for thousands of years in ancient Serbia, China, Egypt, and Greece — moldy bread applied to wounds could prevent or mitigate topical infections.
Penicillin is a purified antibiotic substance derived from specific molds. Discovered in 1928, it was first refined and then mass-produced over the next 15 years. The drug was the first effective treatment for bacterial infections such as pneumonia, and was extraordinarily helpful in combating infection suffered by wounded Allied soldiers during World War 2.
Antibiotics are not harmful to viruses; specific antiviral drugs must be used to combat these pathogens, which are highly susceptible to mutation. Antibiotics will successfully treat bacterial infections present in a patient alongside a viral infection, such as bacterial pneumonia.
To combat the new coronavirus in the year 2020, an experimental antiviral drug remdesivir is being tested presently in China, France, and the United States. The drug targets the polymerase inside a virion; without this enzyme, the virus is unable to replicate itself.
“Because all viruses carry and require one or another version of these enzymes, the hope is that remdesivir, initially developed (not very successfully) for treating Ebola virus infection, may prove effective against the novel coronavirus strain propelling the present pandemic.” — Bruce Goldman, science writer for Stanford University School of Medicine
A vaccine is in the works that will target the protein spikes on the outside of the coronavirus. Coronaviruses typically attach themselves to cells in the upper respiratory tract, but a mutation in SARS-CoV-2 allows its virions to attach themselves via their spikes to an enzyme lining the cells of our lower respiratory tract — part of what makes this pandemic dangerous.
Conclusion
Though there is yet no cure for COVID–19, neither is there a cure for the common cold, an infection of the upper respiratory tract predominantly caused by coronavirus and rhinovirus variants.
Physically distancing oneself from others (who may be infected with the virus and not know it) has been shown to be effective at limiting the transmission of the virus. The best prevention against contracting the virus is refraining from introducing virus particles into one’s body, which is accomplished through touching a contaminated surface and then touching one’s face.
ACE2 enzyme image courtesy of Eric/EMW (CC 3.0), SARS-CoV-2 image (and cover image) courtesy of Scientific Animations (CC 4.0).
Unicorn Riot's COVID–19 Coverage:
- “Brazil is Asking for Help” – Artists and Activists Speak Out - April 10, 2021
- Brazilian Pandemonium: COVID-19 Kills Over 300K - March 27, 2021
- COVID-19 Deaths in Minnesota Prisons Continue to Rise - February 17, 2021
- Brazil Nears 200K Deaths as Politicians Continue to Downplay COVID-19 - December 20, 2020
- Winter of Coronavirus: Seeking Shelter in Minneapolis During COVID–19 - December 14, 2020
- Denver Sweeps 300+ Tent Encampment Residents - November 30, 2020
- Unhoused Community Forms Tenants Union, Constituents Protest at Commissioner’s Home - November 11, 2020
- Minneapolis Prioritizing Park Sweeps Over Sheltering the Unhoused - October 29, 2020
- Court Protest Aims at Boston Covid Housing Crisis - October 29, 2020
- Philly Starbucks Worker Delivers NLRB Unfair Labor Practice Complaint - October 15, 2020
- Demands Reignite for Releases from GEO ICE Jail Amid New Covid Outbreak - October 5, 2020
- Peavey Park Sanctuary Homeless Camp Evicted in Minneapolis - September 24, 2020
- New Month Brings Added Urgency To Minneapolis’ Housing Needs - September 2, 2020
- COVID–19 Testing DeMystified at Community-Informed Coronavirus Testing Site - August 29, 2020
- Sanctuary Camp Residents Pressured to Move, No Housing Solution In Sight - August 22, 2020
- Coronavirus, Corruption, and Resistance: Life Under South Africa’s Lockdown - August 17, 2020
- Authorities Visit Loring Park Tent Encampment, Bring Eviction Scare - August 10, 2020
- Minneapolis Park Police Displace Sanctuary Encampment - July 22, 2020
- Homeless Philadelphians Moving Into Vacant City-Owned Homes - June 22, 2020
- Encampment to ‘Free Them All’ Outside GEO ICE Detention Center - May 26, 2020
- The Coronavirus Crisis in Brazil – An Interview with EmiciThug - May 22, 2020
- Nurses Picket Over Lack of Protection From Ongoing Viral Pandemic - May 21, 2020
- Mutual Aid to Detained Refugee Women Grows — Coronavirus in Greece Part 3 - May 7, 2020
- Minneapolis May Day Protest Supports Essential Workers - May 2, 2020
- MN Demonstrations, Demands to Free Prisoners Escalate - April 30, 2020
- Denver ‘Clean-ups’ Displace 100+ Unhoused Residents Amid Health Crisis - April 30, 2020
- Worker-Occupied Factory Sends Soap to Refugee Camp – Coronavirus in Greece, Part 2 - April 28, 2020
- A Country Quarantined, Coronavirus in Greece Part 1 - April 25, 2020
- Who’s Calling to ‘Liberate Minnesota’, and Why? - April 21, 2020
- Living with COVID–19 - April 17, 2020
- Philly Mayor and Judges Pressured To Release Inmates From Jail - April 15, 2020
- Calls for Rent and Mortgage Freeze Outside MN Legislature - April 14, 2020
- What Is Coronavirus and How Do Humans Defeat It? - April 10, 2020
- Car Protest Demands Philadelphia Officials Release Prisoners To Save Lives In Pandemic Crisis - April 10, 2020
- ‘Cancel Rent’ Demo Calls for a Rent and Mortgage Payment Freeze as COVID-19 Spreads - April 9, 2020
- Coronavirus in the Caribbean: COVID–19 Update from Puerto Rico - April 2, 2020
- ‘Never Again’ Demo Demands Release of Detainees Amidst COVID–19 Pandemic - March 30, 2020
- South Africa Under Lockdown as COVID–19 Spreads - March 29, 2020
- Providing Mutual Aid Amidst the Coronavirus Pandemic in Minnesota’s Twin Cities - March 27, 2020
- As U.S. Coronavirus Cases Top the World Charts, Minnesotans’ “Stay at Home” Order Goes Into Effect - March 27, 2020
- “Everyone Deserves A Cost-Of-Living Adjustment”: Interview with UCSC Striker Yulia Gilich - March 26, 2020
- ‘Real boog hours’: Neo-Nazi Terror and the Coronavirus Crisis - March 20, 2020
- Coronavirus Concerns End St. Paul Educators Strike, Close Many Public Schools - March 14, 2020
Follow us on X (aka Twitter), Facebook, YouTube, Vimeo, Instagram, Mastodon, Threads, BlueSky and Patreon.
Please consider a tax-deductible donation to help sustain our horizontally-organized, non-profit media organization: