Living with COVID–19
St. Paul, MN – The scarcity of coronavirus testing in the United States is significantly impacting the country’s ability to combat the spread of COVID–19. Working- and lower-class people can’t get tested unless they are critically ill. Even frontline health care workers experiencing symptoms are being denied tests due to the nationwide shortage of testing materials.
Unicorn Riot spoke with a Twin Cities blue-collar worker ‘RC’ who has been self-isolating for four weeks since their symptoms began on March 15. Initial symptoms of illness included a bad sore throat, which spread into their lungs, followed by a strong dry cough that persisted for weeks.
They spent hours waiting on the phone to speak to nurses about their symptoms, and have three times gone in to their hospital in an attempt to be tested for COVID–19. They were denied testing all three times; when they went in on April 13, they were told there were no test kits even for influenza.
Seeking testing at hospitals
At first, RC kept trying to find a way to speak with a medical professional without having to physically go in to the hospital. They were deeply worried about infecting other people if they did have COVID–19.
On the phone they spent “hours and hours” on hold at first.
“I got it pretty early on, so it was pretty surprising that it was already that much of a disturbance. Either that or it must have been a lot of people calling in.” — RC
On their second day of symptoms they came across a way to diagnose themselves online. The generic test affirmed that RC likely had COVID–19, and recommended that they self-quarantine for two weeks.
What the test did not offer is a way for RC to get tested at a clinic. (The Mayo Clinic’s assessment claims it will determine if you’re a candidate for a COVID–19 test.)
RC then tried going through their hospital’s online portal, and eventually got ahold of a nurse and requested testing. They were told the same thing — they might have it, so they should quarantine for two weeks. All the while their lungs felt like they were “burning up.”
“I don’t want anyone else to get sick, but I don’t know what permanent damage might be happening or how bad my condition actually is.”
They found out about a new viral clinic at their hospital, where patients were getting screened for coronavirus as well as related or similar infections.
When they went there, medical staff said RC didn’t fit the criteria for testing. RC wasn’t prescribed medication or give any advice aside from ‘stay in quarantine.’
 The University of Minnesota’s medical center is reserving tests only for ‘critically ill’ patients
The University of Minnesota’s medical center is reserving tests only for ‘critically ill’ patients
Their coughing worsened over the next few days, with phlegm beginning to build up in their lungs. When they called the nurse line again, it was recommended they return for testing.
RC told Unicorn Riot the nurse who saw them had said, “It would be really nice to test you because you have a lot of the symptoms.” The nurse added that one of the only ways to get tested is to have been in contact with someone else who has tested positive.
“We both talked about how that’s pretty limited, because there’s definitely people who have contracted it without knowing the person who gave it to them, or that person knowing who gave it to them.“
Chest X-rays were taken on RC’s second visit, and upon examination with a stethoscope the doctor determined it was ‘atypical pneumonia.’ RC was prescribed antibiotics and given a “pretty stern” doctors’ note, which said RC “absolutely was not allowed to go to work.”
RC said the whole experience, especially the not-knowing, has been “pretty frustrating.”
“I don’t know if I’m gonna get better, when I’m gonna get better, if I even have it – if all this missing work, four weeks of missing work is for nothing.“
They’ve finished their antibiotics treatment, but their cough is persisting, as well as soreness and phlegm in their lungs.
On their latest, third visit to the hospital they were told that there were no longer tests available for influenza or for other common viral infections.
The most hospital staff could do was test for mono, despite RC not showing symptoms of that infection. An albuterol inhaler was prescribed to help their breathing.

A clinical lab worker scans barcodes of coronavirus samples in Leeds, England
Image courtesy HM Treasury (CC 2.0)
Facing employer’s skepticism
RC’s workplace has changed their stance over time on RC’s self-quarantining during this pandemic, which they were directed to do by medical professionals.
At first, RC’s manager agreed staying home was a best course of action. As the days went by and RC still hadn’t returned to work, their employer became more vocally skeptical about RC’s illness. “They didn’t think I had it,” said RC, who had been told by medical professionals they very well might have it.
They understand how easily the new coronavirus, SARS-CoV-2 can spread to others, and are very wary of getting anyone else sick.
“I don’t want to be losing money right now. But I’m not gonna risk peoples’ lives for it.“
Managers have begun pressuring RC to come back to work to accomplish tasks “that not a lot of other people can do.”
Though RC’s employer may be considering the consequences of spreading COVID–19 in the workplace, they seem more focused on the loss of revenue “as opposed to thinking about the welfare of the workers there.”
RC added that their employers don’t seem to realize “the fact that we have a lot of older people working where I work.”
“There’s hundreds of people who work there, so if I spread it there, there’s a good chance that a few people would end up dead from that. That is not acceptable, in my mind.“
RC expressed dismay with their employer’s skepticism. Though it’s nice for them to have a break from work, staying home is costing them money. “I would rather be at work than not getting paid.”

Self-quarantining in a shared building
RC said being isolated away from the rest of society, including most of their friends and family, has “been pretty rough.”
“I already have depression, so it does not help — it’s a lot of time in my head. I am getting pretty stir-crazy.“
Living in an apartment building means RC feels they can’t do laundry during quarantine, as the wash room is shared with dozens of others who live in the building.
They reside in a one-bedroom unit with one other person. Though physical distancing is “not really possible” so far their roommate has shown no major symptoms.
Water in their unit was turned off for hours one day with no prior announcement. This was an unpleasant surprise for RC who was reminded it’s currently not possible to “have someone come in” to fix problems in their unit.
“I just feel like I’m in limbo.“
It’s also been hard “to try to figure out how to get groceries;” RC has felt the only justifiable reason to travel while sick is to visit the hospital.
They’ve been posting regular updates to social media about their health. Food has been brought to RC two times by people who know them; the person is buzzed in via the front door, and leaves the bags of supplies in front of the apartment door.
Mutual aid for nurses, by nurses
RC described a project that gives them hope during this unpleasant and uncertain time — a mutual aid effort started by their cousin, who works as a nurse in another state.
Her hospital has a supply of personal protective equipment (PPE) for its nurses while they’re on the clock. When nurses leave the hospital and go home, many don’t have adequate supplies to prevent the virus from passing to their loved ones, “so a lot of nurses are worried about their families getting it.”
RC said that their cousin has been “collecting supplies from the community for her nurses” such as reusable fabric masks, for use to protect their loved ones.
“She’s basically set up a store for them, a free store where people bring in the stuff that they have and it gets distributed to the nurses.“
The free store is set up at the hospital where she works. Nurses can pick it up on their way out the door, then go home and decontaminate themselves with less worry of spreading illness to their family members.
“It’s good to see people taking care of each other, even if the government isn’t doing it very well… that’s good to see,” remarked RC.
State and clinic efforts to combat COVID–19
Minnesota’s stay-at-home order has been extended until May 4, 2020 by order of Governor Tim Walz, who clarified that even if a person feels fine, “you going out may kill someone else’s family. […] We don’t know enough to know about asymptomatic transmission,” people that are carrying the virus yet show no symptoms.
Gov. Walz gave his first address from the State Emergency Operations Center on April 8; he had been self-quarantining from March 24–April 6 after his bodyguard tested positive for coronavirus infection.
The governor said that he expects to see the state continue to add exemptions for workers in businesses such as landscaping, where workers can remain distant from each other and from the public. The MN Department of Agriculture “will write the rules on that.”
He added, “If it were safe, and we could protect people, we would of course start every business tomorrow.”
“Our intention is to save every single life we can.” — Minnesota Governor Tim Walz
The governor also revealed that the Abbott rapid testing kits, of which 15 have been distributed to each state (except Alaska), have enough supplies for only about 100 tests. To re-order supplies for these test kits is “forbidden” by the federal government.
The unavailability of testing materials has reinforced Gov. Walz’ determination to have Minnesota produce its own testing. Rochester’s Mayo Clinic started conducting clinical antibody testing last week, and the University of Minnesota began offering testing in St. Paul on Monday, April 13.
Reportedly the Mayo Clinic has the capacity to produce 10,000 antibody tests per day, in addition to 8,000 diagnostic tests daily. Antibody tests confirm whether somebody has already had coronavirus, and diagnostic tests determine whether somebody is currently infected.
Testing is so limited, health officials estimate that for every confirmed case in Minnesota there are 100 more in the community.
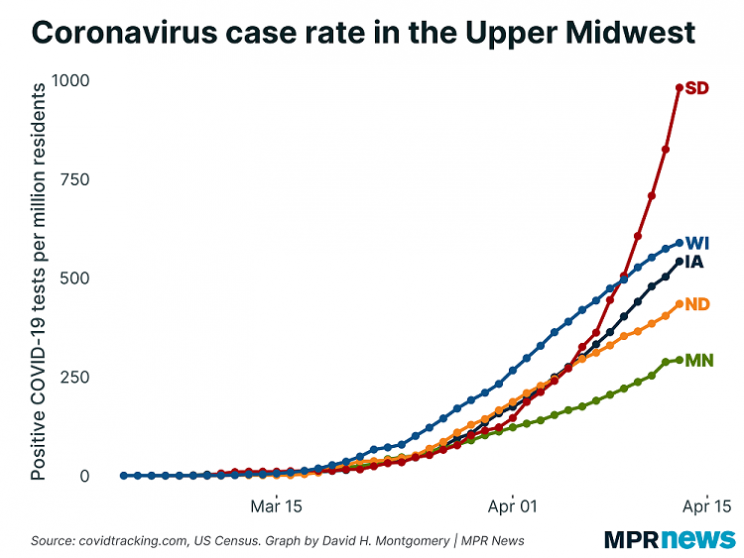
Minnesota has been touting the lowest rates of infection compared with surrounding states in the upper Midwest. Gov. Walz re-emphasized how vital it was to follow the stay-at-home order and maintain distance from each other during the pandemic, and congratulated Minnesotans on having done well so far.
RC told Unicorn Riot that they hope people take the pandemic threat seriously. Even in places where local governments aren’t ordering residents to self-isolate, “they should do it, ’cause we want to stop the spread as much as possible.”
“Even though everyone will eventually probably get it, at least we won’t overwhelm the hospitals as much. ‘Cause they are definitely being overwhelmed, even in our state which isn’t being hit that hard right now.“
More information continues to be learned about the new coronavirus and the ongoing pandemic. As there is yet no vaccine or ‘cure’ for COVID–19, Minnesotans and those in surrounding states would be best served by continuing to remain physically-distant from each other.
Cover image background (3D model of Coronavirus spike protein structure) courtesy of National Institutes of Health (CC 2.0)
Unicorn Riot's COVID–19 Coverage:
- “Brazil is Asking for Help” – Artists and Activists Speak Out - April 10, 2021
- Brazilian Pandemonium: COVID-19 Kills Over 300K - March 27, 2021
- COVID-19 Deaths in Minnesota Prisons Continue to Rise - February 17, 2021
- Brazil Nears 200K Deaths as Politicians Continue to Downplay COVID-19 - December 20, 2020
- Winter of Coronavirus: Seeking Shelter in Minneapolis During COVID–19 - December 14, 2020
- Denver Sweeps 300+ Tent Encampment Residents - November 30, 2020
- Unhoused Community Forms Tenants Union, Constituents Protest at Commissioner’s Home - November 11, 2020
- Minneapolis Prioritizing Park Sweeps Over Sheltering the Unhoused - October 29, 2020
- Court Protest Aims at Boston Covid Housing Crisis - October 29, 2020
- Philly Starbucks Worker Delivers NLRB Unfair Labor Practice Complaint - October 15, 2020
- Demands Reignite for Releases from GEO ICE Jail Amid New Covid Outbreak - October 5, 2020
- Peavey Park Sanctuary Homeless Camp Evicted in Minneapolis - September 24, 2020
- New Month Brings Added Urgency To Minneapolis’ Housing Needs - September 2, 2020
- COVID–19 Testing DeMystified at Community-Informed Coronavirus Testing Site - August 29, 2020
- Sanctuary Camp Residents Pressured to Move, No Housing Solution In Sight - August 22, 2020
- Coronavirus, Corruption, and Resistance: Life Under South Africa’s Lockdown - August 17, 2020
- Authorities Visit Loring Park Tent Encampment, Bring Eviction Scare - August 10, 2020
- Minneapolis Park Police Displace Sanctuary Encampment - July 22, 2020
- Homeless Philadelphians Moving Into Vacant City-Owned Homes - June 22, 2020
- Encampment to ‘Free Them All’ Outside GEO ICE Detention Center - May 26, 2020
- The Coronavirus Crisis in Brazil – An Interview with EmiciThug - May 22, 2020
- Nurses Picket Over Lack of Protection From Ongoing Viral Pandemic - May 21, 2020
- Mutual Aid to Detained Refugee Women Grows — Coronavirus in Greece Part 3 - May 7, 2020
- Minneapolis May Day Protest Supports Essential Workers - May 2, 2020
- MN Demonstrations, Demands to Free Prisoners Escalate - April 30, 2020
- Denver ‘Clean-ups’ Displace 100+ Unhoused Residents Amid Health Crisis - April 30, 2020
- Worker-Occupied Factory Sends Soap to Refugee Camp – Coronavirus in Greece, Part 2 - April 28, 2020
- A Country Quarantined, Coronavirus in Greece Part 1 - April 25, 2020
- Who’s Calling to ‘Liberate Minnesota’, and Why? - April 21, 2020
- Living with COVID–19 - April 17, 2020
- Philly Mayor and Judges Pressured To Release Inmates From Jail - April 15, 2020
- Calls for Rent and Mortgage Freeze Outside MN Legislature - April 14, 2020
- What Is Coronavirus and How Do Humans Defeat It? - April 10, 2020
- Car Protest Demands Philadelphia Officials Release Prisoners To Save Lives In Pandemic Crisis - April 10, 2020
- ‘Cancel Rent’ Demo Calls for a Rent and Mortgage Payment Freeze as COVID-19 Spreads - April 9, 2020
- Coronavirus in the Caribbean: COVID–19 Update from Puerto Rico - April 2, 2020
- ‘Never Again’ Demo Demands Release of Detainees Amidst COVID–19 Pandemic - March 30, 2020
- South Africa Under Lockdown as COVID–19 Spreads - March 29, 2020
- Providing Mutual Aid Amidst the Coronavirus Pandemic in Minnesota’s Twin Cities - March 27, 2020
- As U.S. Coronavirus Cases Top the World Charts, Minnesotans’ “Stay at Home” Order Goes Into Effect - March 27, 2020
- “Everyone Deserves A Cost-Of-Living Adjustment”: Interview with UCSC Striker Yulia Gilich - March 26, 2020
- ‘Real boog hours’: Neo-Nazi Terror and the Coronavirus Crisis - March 20, 2020
- Coronavirus Concerns End St. Paul Educators Strike, Close Many Public Schools - March 14, 2020
Follow us on X (aka Twitter), Facebook, YouTube, Vimeo, Instagram, Mastodon, Threads, BlueSky and Patreon.
Please consider a tax-deductible donation to help sustain our horizontally-organized, non-profit media organization:


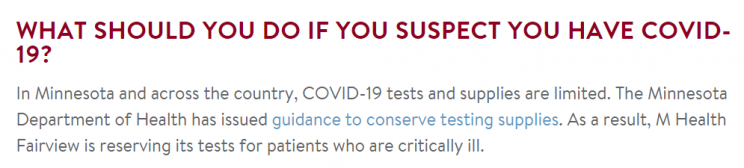 The University of Minnesota’s medical center is reserving tests only for ‘critically ill’ patients
The University of Minnesota’s medical center is reserving tests only for ‘critically ill’ patients
